Read time 6 minutes
First off, thank you, Universe. Every day I wake up feeling blessed. Recovery isn’t linear, and neither is health, but both are worth fighting for. If you’re reading this blog, welcome to my world of reflection, resilience, and plenty of research.
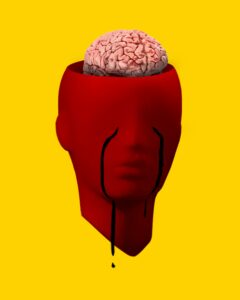
Living with the Unseen: The Fine Line Between Health and Illness

There’s a strange, often misunderstood space where many chronically ill people exist. It is a zone that’s neither fully healthy nor visibly sick. It’s a place where symptoms persist, but validation remains elusive.
Living with an invisible illness like Isaacs’ Syndrome has meant facing two battles: one with my body, and one with the world around me. From the outside, I may look fine, no casts, no scars, no visible signs of struggle. But inside, my body wages a relentless battle against itself.
I am no longer confined to a hospital bed, but I’m not scaling mountains either. My body is in quiet rebellion, yet my face still smiles.
This is the space I’ve occupied since 2014. I was sick enough to suffer, but not ill enough to be believed.
That year, my life took a sharp turn. I was diagnosed with Isaacs’ Syndrome. It is a rare neurological disorder characterized by continuous muscle fiber activity. Imagine your muscles twitching, spasming, and refusing to rest, day and night. It’s like your body is constantly whispering, “I’m not okay,” even when the world expects you to be.
But Isaacs’ Syndrome was just the beginning of a long, complicated medical journey.
Layer Upon Layer: The Avalanche of Diagnoses

Shortly after, I was diagnosed with Lyme disease. It is a bacterial infection transmitted through tick bites. Lyme is infamous for its stealth, it mimics other conditions, hides in tissues, and often goes undetected for years. For me, it added another layer of fatigue, joint pain, and neurological confusion.
Then came Glaucoma, silently threatening my vision. And Membranous Glomerulonephritis. It is a kidney condition that made me rethink every sip of water and every bite of food.
As if my body had become a magnet for medical mysteries, more conditions followed like uninvited guests:
| Condition | Impact |
|---|---|
| Irritable Bowel Syndrome (IBS) | Unpredictable digestion, chronic discomfort |
| Diabetes | Constant blood sugar monitoring, dietary restrictions |
| Frozen Shoulder | Limited mobility, persistent pain |
| Eczema | Skin inflammation, itching, flare-ups |
| Blood Pressure issues | Dangerous fluctuations, fatigue |
Each diagnosis chipped away at the illusion of normalcy. Yet, to the outside world, I looked fine. I smiled. I worked. I showed up. And that’s where the real struggle began.
“But You Don’t Look Sick”: The Invalidation of Invisible Illness

Because my symptoms aren’t visible, they’re often dismissed or doubted. I’ve been told to “just push through it., “try yoga,” or “get more sleep,” as if my condition were a lifestyle choice rather than a neurological reality.
If I had a dollar for every time someone said, “But you don’t look sick,” I could probably fund my own research lab. This phrase, often said with good intentions, feels like a slap in the face to those living with invisible illnesses.
What people don’t see are the sleepless nights. The medication side effects. The mental gymnastics of managing symptoms, appointments, and uncertainty. They don’t see the pain behind the smile, the fatigue behind the laughter, or the anxiety behind the silence.
Invisible illness is a paradox.
I am constantly battling something that others can’t see, and often, don’t believe.
The Psychological Toll of Being Disbelieved
Living in this space affects more than just the body, it takes a toll on the mind. The constant need to explain, justify, and prove your pain is exhausting.
The public challenges have been just as difficult as the private ones. I’ve faced skepticism from colleagues, friends, and even healthcare professionals. I’ve had to advocate for myself repeatedly, explaining a disease most people have never heard of. I’ve missed opportunities, been judged unfairly, and felt the sting of being labeled “lazy” or “dramatic.”
There was a time when I began questioning myself: Am I exaggerating? Is it really that bad? Should I just push through?
This internalized doubt is a form of gaslighting. It is often reinforced by society, workplaces, and even healthcare providers. When my symptoms didn’t fit neatly into a diagnostic box, I was labeled as anxious, dramatic, or attention-seeking.
But here’s the truth: invisible doesn’t mean imaginary.
The Complexity of Chronic Conditions

One of the hardest parts of living with multiple chronic illnesses is the complexity. Each condition interacts with the others in unpredictable ways:
- Treating one can worsen another
- Medications clash
- Symptoms overlap
It’s a constant balancing act.
For example:
- Managing diabetes requires dietary control, but IBS makes that nearly impossible.
- Treating glaucoma involves eye drops that can trigger eczema.
- Isaacs’ Syndrome causes muscle twitching that worsens with stress. This stress is inevitable when juggling so many health issues.
There’s no one-size-fits-all solution. Every day is a new puzzle, and every decision feels like a gamble.
Coping Mechanisms: Finding Peace in Chaos

Despite the chaos, I’ve found strategies that help me navigate this unpredictable terrain. These aren’t miracle cures, they’re lifelines.
1. Acceptance
Instead of fighting my reality, I’ve learned to accept it. That doesn’t mean giving up—it means acknowledging what is and working from there. Acceptance has brought clarity and peace.
2. Mindfulness & Meditation
These practices help me stay grounded, especially during flare-ups. A few minutes of deep breathing can make a world of difference when your body feels like it’s falling apart.
3. Advocacy
Speaking up about my conditions has been empowering. Whether it’s educating others or pushing for better care, advocacy gives me a sense of purpose. It transforms pain into progress.
4. Community Support
Connecting with others who live in the same space has been life changing.
We validate each other in ways the world often doesn’t. Online forums, support groups, and social media became safe havens.
Why I Felt The Need to Talk About This

The conversation around chronic illness needs to evolve.
Together, we must move beyond the binary of “sick” and “healthy” and recognize the spectrum of health and the millions who live in the in-between.
What Needs to Change:
- Employers must accommodate invisible disabilities with empathy and flexibility.
- Educators should be trained to recognize and support students with chronic conditions.
- Healthcare providers must listen without judgment and treat patients as partners.
- Friends and family must learn to support without needing visual proof.
Society must understand that wellness isn’t always visible. Just because someone looks okay doesn’t mean they are.
Final Thoughts: Redefining Strength
Strength isn’t just about lifting weights or running marathons.
For me, strength is:
- Getting out of bed when my body feels like lead
- Attending a meeting while my muscles twitch uncontrollably
- Smiling when my kidneys ache and my blood sugar spikes
Living with invisible illness has taught me that resilience isn’t loud. It’s quiet. It’s deeply personal. It’s the kind of strength that doesn’t need applause; it just needs acknowledgment.
So, the next time someone says, “But you don’t look sick,” I’ll smile and say, “That’s because you’re not looking deep enough.”
DISCLAIMER
The views expressed in this article are my own and do not constitute medical advice. Please consult a healthcare professional for any health-related concerns.


